| Name | Cytarabine |
| Classes |
Anticancer/Antineoplastic Agent Antimetabolites |
| Diseases |
Cancer Leukemia Meningitis |
Cytarabine
Cytarabine is antineoplastic drug from the class antimetabolites. Cytarabine acts through the inhibition of DNA polymerase. A limited, but significant, incorporation of cytarabine into both DNA and RNA has also been reported. Extensive chromosomal damage, including chromatoid breaks, have been produced by cytarabine and malignant transformation of rodent cells in culture has been reported. Deoxycytidine prevents or delays (but does not reverse) the cytotoxic activity.
Cytarabine Injection in combination with other approved anti-cancer drugs is indicated for-
- remission induction in acute non-lymphocytic leukemia of adults and pediatric patients
- treatment of acute lymphocytic leukemia
- chronic myelocytic leukemia
- meningeal leukemia
In the induction therapy of acute non-lymphocytic leukemia, the usual cytarabine dose in combination with other anti-cancer drugs is 100 mg/m2/day by continuous intravenous infusion (Days 1-7) or 100 mg/m2 intravenous every 12 hours (Days 1-7).
Intrathecal Use in Meningeal Leukemia
Cytarabine injection has been used intrathecally in acute leukemia in doses ranging from 5 mg/m2 to 75 mg/m2 of body surface area. The frequency of administration varied from once a day for 4 days to once every 4 days. The most frequently used dose was 30 mg/m2 every 4 days until cerebrospinal fluid findings were normal, followed by one additional treatment. The dosage schedule is usually governed by the type and severity of central nervous system manifestations and the response to previous therapy.
The most common adverse reactions of cytarabine are-
- anorexia
- nausea
- vomiting
- diarrhea
- oral and anal inflammation or ulceration
- hepatic dysfunction
- fever
- rash
- thrombophlebitis
- bleeding
- Only cancer chemotherapy specialists should use Cytarabine Injection.
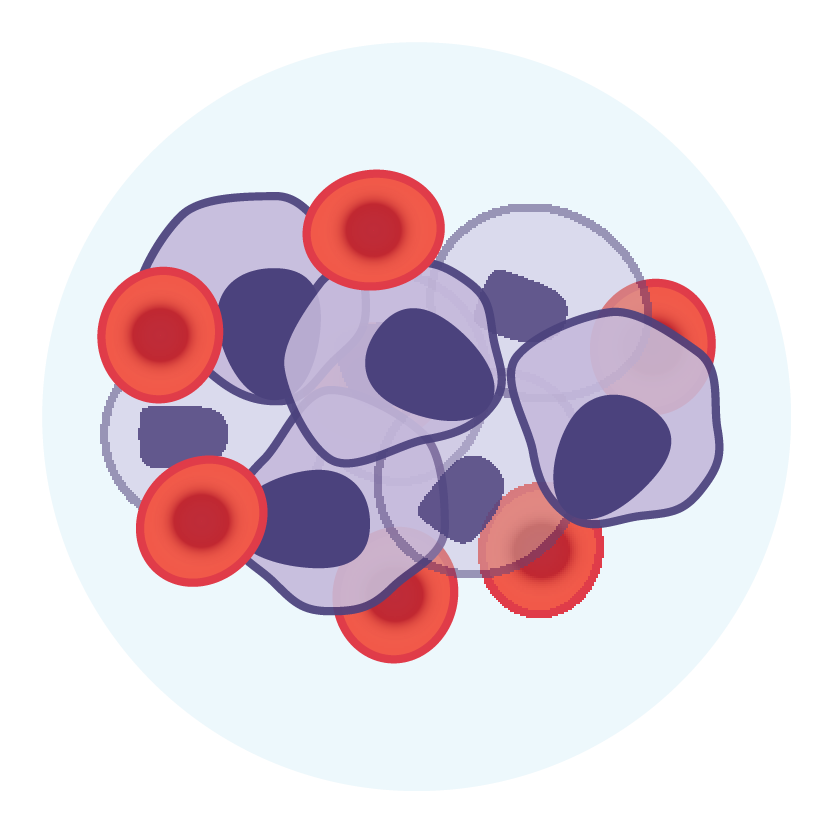
- Patients undergoing induction therapy should be treated in a facility with sufficient laboratory and supportive resources to monitor drug tolerance and protect and maintain a patient compromised by drug toxicity. The main toxicity of cytarabine injection is bone marrow suppression, which includes leukopenia, thrombocytopenia, and anemia. Less severe toxicity symptoms include nausea, vomiting, diarrhea, and abdominal pain, as well as oral ulceration and hepatic dysfunction.
- Cytarabine is a highly effective bone marrow suppressant. In patients with a history of drug-induced bone marrow suppression, therapy should be initiated with caution. Patients taking this medication must be closely monitored by a doctor and have daily leucocyte and platelet counts performed during induction therapy.
- Following some experimental dose schedules for cytarabine injection, severe and sometimes fatal CNS, GI, and pulmonary toxicity (different from that seen with conventional therapy regimens of cytarabine injection) has been reported.
- Following experimental high dose therapy with cytarabine in combination with cyclophosphamide when used for bone marrow transplant preparation, cases of cardiomyopathy with subsequent death have been reported.
- Following experimental high dose therapy with cytarabine used for the treatment of relapsed leukemia at one institution, 16/72 patients developed a syndrome of sudden respiratory distress, rapidly progressing to pulmonary edema, and radiographically pronounced cardiomegaly. This syndrome has the potential to be fatal.
- When Cytarabine Injection is given to a pregnant woman, it can harm the fetus. Cytarabine is teratogenic to the rat fetus and causes abnormal cerebellar development in neonatal hamsters. In pregnant women, there are no adequate and well-controlled studies. Women of childbearing age should be advised to avoid pregnancy.
Contraindication
Contraindicated in patients hypersensitive to cytarabine or any component of the formulation.
None known.
Contraindicated in pregnancy.
 Bangla
Bangla English
English